INSOMNIA
What to do if you have insomnia or restless sleep?
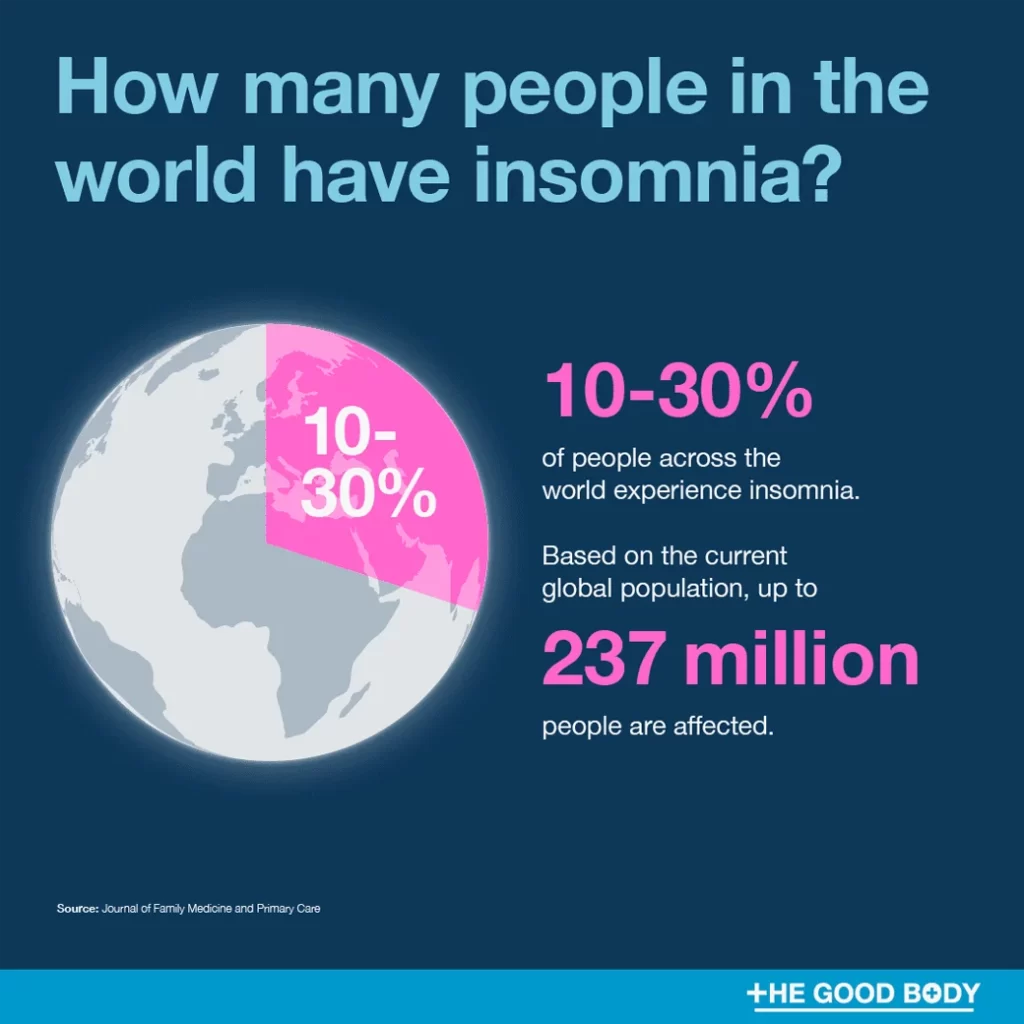
Sleep Problems: A Growing Global Health Concern Sleep disturbances—especially insomnia and restless sleep—are becoming a major public health concern in both Thailand and across the globe. These issues significantly affect physical health, mental well-being, and quality of life.
According to the Thai Ministry of Public Health’s Department of Mental Health, 1 in 3 Thais experience sleep-related problems. Common triggers include stress, anxiety, poor mental health, and lifestyle factors like late-night screen use and caffeine consumption.
Globally, the World Health Organization (WHO) reports that 1 in 4 people suffer from sleep issues, with the problem especially pronounced in developed countries due to fast-paced living and work-related stress. While developing nations show lower rates, the numbers are steadily increasing.
Table of Contents
10 Common Causes and Risk Factors of Insomnia
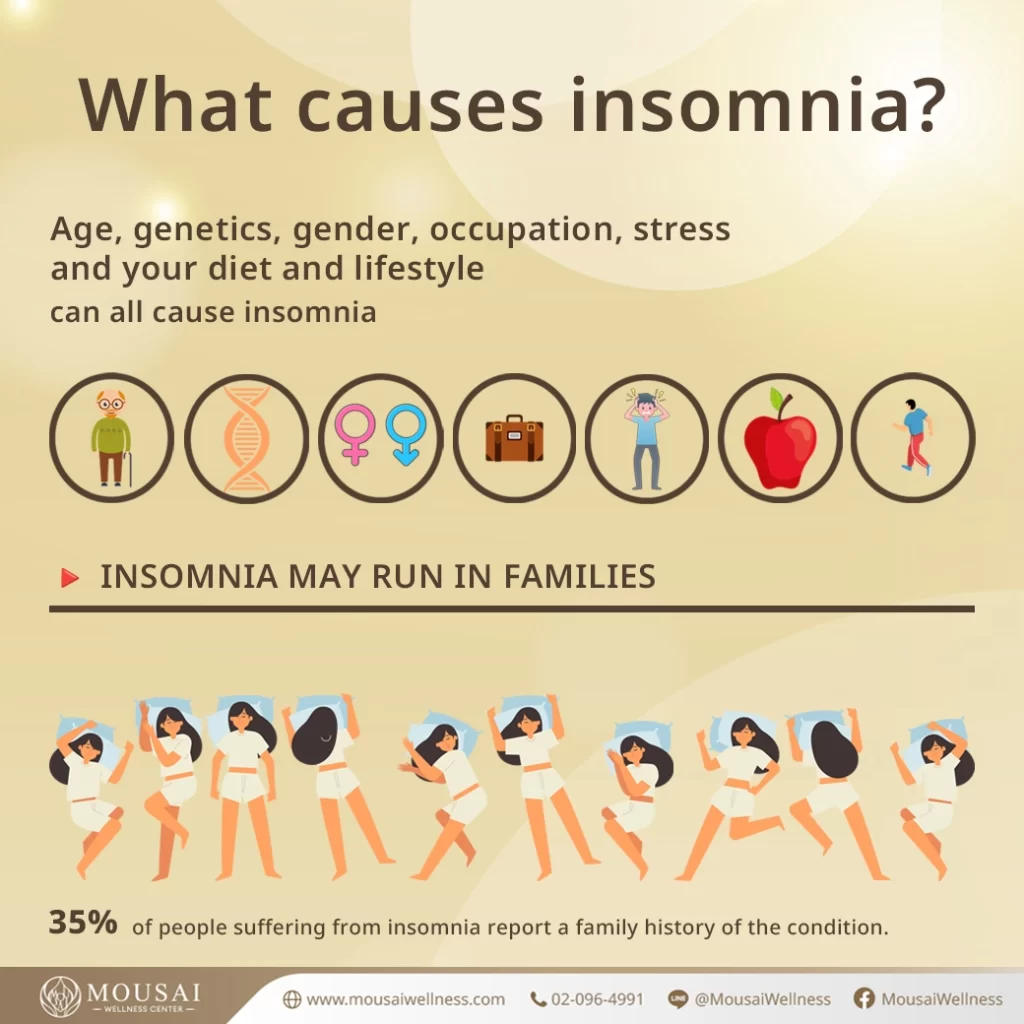
- Fast-paced lifestyle: Constant mental activity and multitasking trigger anxiety and disrupt sleep.
- Excessive screen time: Blue light from phones and tablets interferes with melatonin production.
- Chronic stress: Worries related to work, finances, or family can keep the mind overly alert.
- Mood disorders: Especially depression and anxiety.
- Gender differences: Women are statistically more likely to suffer from insomnia.
- Ageing: Sleep quality often declines with age.
- Hormonal imbalances: Affecting the sleep-wake cycle.
- Chronic illness: Conditions like diabetes, pain, and high blood pressure often impact sleep.
- Other sleep disorders: Restless leg syndrome (RLS), sleep apnea, and more.
- Genetics: A family history of insomnia increases your likelihood.
Hormones Related to Sleep
Hormones play an important role in regulating the body’s sleep-wake cycle. Abnormal levels of these hormones can cause sleep problems such as insomnia, frequent waking, or insufficient rest. Therefore, maintaining hormonal balance is crucial for quality sleep and good health.
1. Melatonin Hormone – The Sleep Hormone 🛌
Melatonin is produced by the pineal gland in our brain and is released at night. It prepares the body for sleep by making us feel sleepy, lowering body temperature, and slowing down the central nervous system. Additionally, melatonin has antioxidant properties, which help slow aging and reduce the risk of cancer. Truly fortunate!
2. Cortisol Hormone 😡
Cortisol is the hormone responsible for managing stress. When the body experiences stress, cortisol levels increase, causing feelings of restlessness and poor sleep quality. Therefore, reducing stress is essential for good sleep. Exercise and relaxation before bedtime also help regulate cortisol levels—helping you relieve stress and sleep better at the same time!
3. Growth Hormone 🌃
Growth hormone plays a role in regulating sleep in women, especially during their menstrual cycle. Because this hormone peaks just before menstruation, it can cause insomnia more easily. Additionally, symptoms such as chills, headaches, and mood swings—related to growth hormone fluctuations—can also lead to restless sleep. Ways to relieve these symptoms include exercising, drinking herbal tea, or getting a relaxing massage before bedtime to help the body rest adequately.
4. Oxytocin Hormone – The Love Hormone🎎
Oxytocin plays a role in both sleep and love.
5 Thyroid Hormone 🦋
When there is a deficiency of thyroxine, a key hormone produced by the thyroid gland, the body may feel fatigued, weak, depressed, and experience mood swings, along with sleep problems. This is because thyroid hormone helps regulate sleep and wakefulness. A lack of thyroid hormone can cause difficulty falling asleep or even temporary breathing pauses during sleep.
6. Estrogen Hormone 👩🦰
Estrogen is a female sex hormone with multiple roles. If its levels are abnormally high, it may cause insomnia or restless sleep because it suppresses the function of melatonin, the hormone that regulates sleep. Additionally, it can cause symptoms such as restlessness, stress, anxiety, and poor-quality sleep.
Management methods include taking prescribed thyroid hormone (thyroxine) supplements as directed by a doctor, as well as adjusting sleep habits. For example, exercising regularly, avoiding stimulants before bedtime, and getting enough rest can help improve sleep quality.
Managing this condition may require hormone balance adjustment or treatment by a specialist, along with behavioral changes such as regular exercise, avoiding stimulants, and maintaining a consistent sleep routine to allow the body to rest fully and improve quality of life.
Effects of Insomnia on Health

Sleep is an essential activity for human survival as it allows the body and mind to rest and recover. However, insomnia has become an important health issue in modern society, affecting both physical and mental health.
Physical Effects of Insomnia
- Weakened Immune System: Lack of sleep reduces the levels of hormones that regulate the immune system, increasing the body’s susceptibility to infections. Research has found that people who sleep less than 7 hours per day are three times more likely to catch a cold (Prather et al., 2015).
- Increased Risk of Chronic Diseases: Insufficient sleep causes long-term stress on the body, raising cortisol and blood sugar levels, which increases the risk of obesity, diabetes, and heart disease (Buxton & Marcelli, 2010).
- Higher Rates of Accidents and Errors: Sleepiness reduces problem-solving ability and memory. Work performance decreases by about 20% in those who sleep less than 6 hours per night (Lim & Dinges, 2010).
Psychological Impacts of Insomnia
- Increased Risk of Depression: Research shows that individuals who sleep less than 5 hours per night on a regular basis are 2.8 times more likely to experience depression compared to those who sleep more than 8 hours (Zhai et al., 2015).
- Greater Mood Instability: Inadequate sleep leads to hormonal imbalances that regulate mood, resulting in increased irritability, emotional instability, and difficulty controlling emotions (Minkel et al., 2012).
- Impact on Dementia Risk: Studies have shown that consistent, sufficient sleep is associated with a reduced risk of developing dementia, as it helps maintain long-term cognitive functioning (Scullin & Bliwise, 2015).
Chronic insomnia can severely impact mental health and overall well-being. Therefore, addressing sleep problems is essential. This includes adjusting sleep habits, avoiding sleep-disrupting factors, and following good sleep hygiene practices to minimize the negative consequences of inadequate rest.
Lack of Sleep Does Not Directly Cause Obesity
Nowadays, overweight and obesity have become a global public health concern. Besides behavioral factors such as diet and exercise, insufficient sleep is also significantly linked to these conditions. Sleep is a crucial process for regulating hormones involved in metabolism and appetite control. When sleep is disturbed, the body’s systems become imbalanced, potentially leading to overweight and obesity.
One of the main mechanisms connecting insomnia and obesity involves the hormone leptin, which plays a key role in controlling hunger and appetite. Research has found that insufficient sleep causes the body to become resistant to leptin’s effects, leading to increased feelings of hunger and difficulty controlling food intake (Shubham et al., 2015).

In addition, insufficient sleep increases the level of cortisol, a hormone related to stress management. High cortisol levels contribute to the accumulation of abdominal fat and accelerate the process of fat creation. A study by Kumari et al. (2009) found that individuals who sleep less than 6 hours per night have cortisol levels 50% higher than the control group.
Insufficient sleep also affects the function of melatonin, a hormone produced in the sleep cycle that is involved in energy metabolism. Lack of melatonin leads to decreased energy expenditure. Combined with the fact that sleep deprivation itself lowers energy expenditure, this contributes to the problem of maintaining excess body weight (Gonnissen et al., 2013).
Sleep disturbances may also lead to changes in eating patterns. Research by Greer et al. (2013) found that people who sleep less tend to consume more carbohydrates, saturated fats, and sugary foods than usual, ultimately leading to excess energy storage.
Beyond hormonal and physiological mechanisms, insufficient sleep negatively impacts behaviors associated with obesity, such as reduced self-control, increased emotional eating, lack of motivation to exercise, and sedentary lifestyles. All of these are significant risk factors for overweight and obesity (Panossian & Veasey, 2012).
A large body of current research supports a causal relationship between insufficient sleep and the development of overweight and obesity, emphasizing the importance of healthy sleep in weight management and sustainable obesity prevention.
Therefore, raising awareness about sleep problems and improving sleep quality are essential components in maintaining balance and overall health.
Adrenal Fatigue: A Major Cause of Insomnia
Adrenal fatigue is a condition where the body faces chronic stress, causing the adrenal glands to overwork, leading to severe fatigue and exhaustion. Many people may be surprised to learn that sleep behaviors can affect adrenal gland function and contribute to this condition. When sleep problems occur—whether from insufficient sleep or poor sleep quality—the body experiences chronic stress due to lack of rest and inadequate recovery, resulting in an overworked endocrine system, particularly the adrenal glands.
The adrenal glands play a crucial role in producing hormones that respond to stress, primarily cortisol. When the body lacks sufficient sleep, cortisol levels become abnormally high. Prolonged high cortisol levels can exceed the adrenal glands’ capacity to cope, eventually leading to adrenal fatigue.
Research by Leproult et al. (1997) found that sleeping less than 4 hours per night for six consecutive days increased cortisol levels by 37% compared to those who slept 8 hours. Additionally, Wright et al. (2015) reported that people who regularly sleep less than 5 hours per night have a 45% higher risk of developing adrenal fatigue.
Insomnia also contributes to dysfunction in various other hormones beyond cortisol, including growth hormone, thyroid hormone, and insulin. Dysregulation of these hormones further exacerbates the symptoms of adrenal fatigue, such as insomnia, mood swings, loss of appetite, stress, anxiety, and weakness (Marcelle, 2015).
Other potential consequences of untreated adrenal fatigue include unintended weight loss, memory impairment, worsening insomnia, neck and upper back pain, and high blood pressure (Wilson, 2001).
Therefore, maintaining good sleep quality is a critical factor in preventing adrenal fatigue. This can be achieved by establishing a consistent sleep routine, getting adequate rest, avoiding sleep disturbances, managing stress before bedtime, and consulting a healthcare professional if severe sleep problems persist. These steps help prevent serious long-term health complications.
Insomnia Symptoms Caused by Low Thyroid Hormone Levels
Thyroid hormones play a crucial role in regulating the body’s sleep patterns. Therefore, when there is an abnormality in thyroid hormone levels, especially in conditions with low thyroid hormone or hyperthyroidism, various sleep problems can arise.
The key thyroid hormone involved in sleep regulation is thyroxine, which is produced by the thyroid gland. Thyroxine is responsible for controlling the body’s natural sleep-wake cycle. When the level of this hormone is abnormal, it directly affects sleep quality.
In cases of thyroxine deficiency, the central nervous system does not function optimally, and the activity of other hormones related to sleep also becomes disrupted. This results in insomnia symptoms, which have been reported in 57-64% of patients with hyperthyroidism (Wichaidit et al., 2021).
Insomnia symptoms caused by hyperthyroidism include difficulty falling asleep (insomnia), non-restorative sleep, insufficient deep sleep, poor sleep quality, sleep-disordered breathing, and feeling unrefreshed upon waking even after a long sleep duration (Dikmetash et al., 2022).
Research indicates that hyperthyroidism is associated with abnormalities in neurotransmitter feedback mechanisms in the brain that regulate sleep. For example, the activity of serotonin neurotransmitters increases during sleep but decreases during wakefulness, which is a key mechanism causing insomnia in people with hyperthyroidism (Dikmetash et al., 2022).
Additionally, hyperthyroidism is linked to abnormal functioning of melatonin, a hormone produced by the body in a daily cycle to regulate the sleep-wake rhythm. People with hyperthyroidism have reduced melatonin levels in their bloodstream, leading to poorer sleep quality (Rahman et al., 2016).
Besides causing fatigue, insomnia also negatively affects physical and mental health. Studies have found that people with hyperthyroidism who suffer from insomnia are at a higher risk of depression, mental health problems, aggressive behavior, and impairments in memory and attention (Ness-Abramof et al., 2010).
To manage insomnia in hyperthyroid patients, treatment should first focus on resolving the hyperthyroid condition, often requiring antithyroid medications according to treatment guidelines. Afterwards, improving sleep hygiene and behavior is recommended, such as maintaining a consistent sleep schedule, avoiding sleep disturbances, and practicing stress-relief techniques before bedtime. If insomnia persists, specialized treatment from a medical expert may be necessary.
แพ็คเกจ การตรวจฮอร์โมน

References :
– Buxton, O. M., & Marcelli, E. (2010). Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Social Science & Medicine, 71(5), 1027-1036.
– Lim, J., & Dinges, D. F. (2010). A meta-analysis of the impact of short-term sleep deprivation on cognitive variables. Psychological Bulletin, 136(3), 375-389.
– Minkel, J., Moreta, M., Muto, J., Htaik, O., Jones, C., Basner, M., & Dinges, D. (2012). Sleep deprivation potentiates HPA axis stress reactivity in healthy adults. Health Psychology, 33(11), 1430–1434.
– Prather, A. A., Janicki-Deverts, D., Hall, M. H., & Cohen, S. (2015). Behaviorally assessed sleep and susceptibility to upper respiratory illness. Sleep, 38(9), 1497.
– Scullin, M. K., & Bliwise, D. L. (2015). Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspectives on Psychological Science, 10(1), 97-137.
– Zhai, L., Zhang, H., & Zhang, D. (2015). Sleep duration and depression among adults: A meta‐analysis of prospective studies. Depression and Anxiety, 32(9), 664-670.
– Leproult, R., Copinschi, G., Buxton, O., & Van Cauter, E. (1997). Sleep loss results in an elevation of cortisol levels the next evening. Sleep, 20(10), 865-870.
– Marcelle, G. (2015). Chronic fatigue and hormones. Australian Family Physician, 44(4), 166-167.
– Wilson, J.L. (2001). Adrenal Fatigue: The 21st Century Stress Syndrome. Smart Publications.
– Wright Jr, K. P., Drake, A. L., Frey, D. J., Fleshner, M., Desouza, C. A., Gronfier, C., & Czeisler, C. A. (2015). Influence of sleep deprivation and circadian misalignment on cortisol, inflammatory markers, and cytokine balance. Brain, Behavior, and Immunity, 47, 24-34.
เอกสารอ้างอิง :
Gonnissen, H. K., Hulshof, T., Westerterp-Plantenga, M. S. (2013). Chronobiology